Обнаружение и высокое содержание ДНК герпесвирусов (Orthoherpesviridae) в аутопсийных материалах пациентов с летальным исходом COVID-19
- Авторы: Юрлов К.И.1, Якушина С.А.1,2, Федорова Н.Е.1, Кистенева Л.Б.1,2, Келли Е.И.2, Каниболоцкий А.А.3,4, Ивкин Е.Н.3,4, Антипят Н.А.2, Тюрин И.Н.2, Ларичев В.Ф.1, Демидова Н.А.1, Леснова Е.И.1, Климова Р.Р.1, Масалова О.В.1, Кущ А.А.1
-
Учреждения:
- ФГБУ «Национальный исследовательский центр эпидемиологии и микробиологии имени Н.Ф. Гамалеи» Минздрава России
- ГБУЗ «Инфекционная клиническая больница № 1 ДЗМ»
- ГБУЗ «Научно-исследовательский институт скорой помощи им. Н.В. Склифосовского ДЗМ»
- ГБУ «Научно-исследовательский институт организации здравоохранения и медицинского менеджмента ДЗМ»
- Выпуск: Том 69, № 2 (2024)
- Страницы: 134-150
- Раздел: ОРИГИНАЛЬНЫЕ ИССЛЕДОВАНИЯ
- URL: https://ogarev-online.ru/0507-4088/article/view/256875
- DOI: https://doi.org/10.36233/0507-4088-215
- EDN: https://elibrary.ru/jxmqzh
- ID: 256875
Цитировать
Полный текст
Аннотация
Введение. Вирус SARS-CoV-2 вызывает нарушения иммунитета, создающие условия для реактивации герпесвирусов человека (ГВЧ). Однако влияние ГВЧ на течение и исход COVID-19 оценивается неоднозначно.
Цель исследования – изучение возможной связи между реактивацией ГВЧ у пациентов, инфицированных SARS-CoV-2, и неблагоприятным исходом COVID-19.
Материалы и методы. Посмертные клинические материалы из головного мозга, печени, селезенки, лимфоузлов и легких были получены от 59 пациентов, находившихся на лечении в ГБУЗ ИКБ № 1 ДЗ г. Москвы в 2021–2023 гг. В 1-ю группу включили материалы от 39 пациентов с летальным исходом COVID-19; во 2-ю группу – от 20 пациентов, не инфицированных SARS-CoV-2 и умерших от разных соматических заболеваний. ДНК ГВЧ и РНК SARS-CoV-2 определяли методом ПЦР.
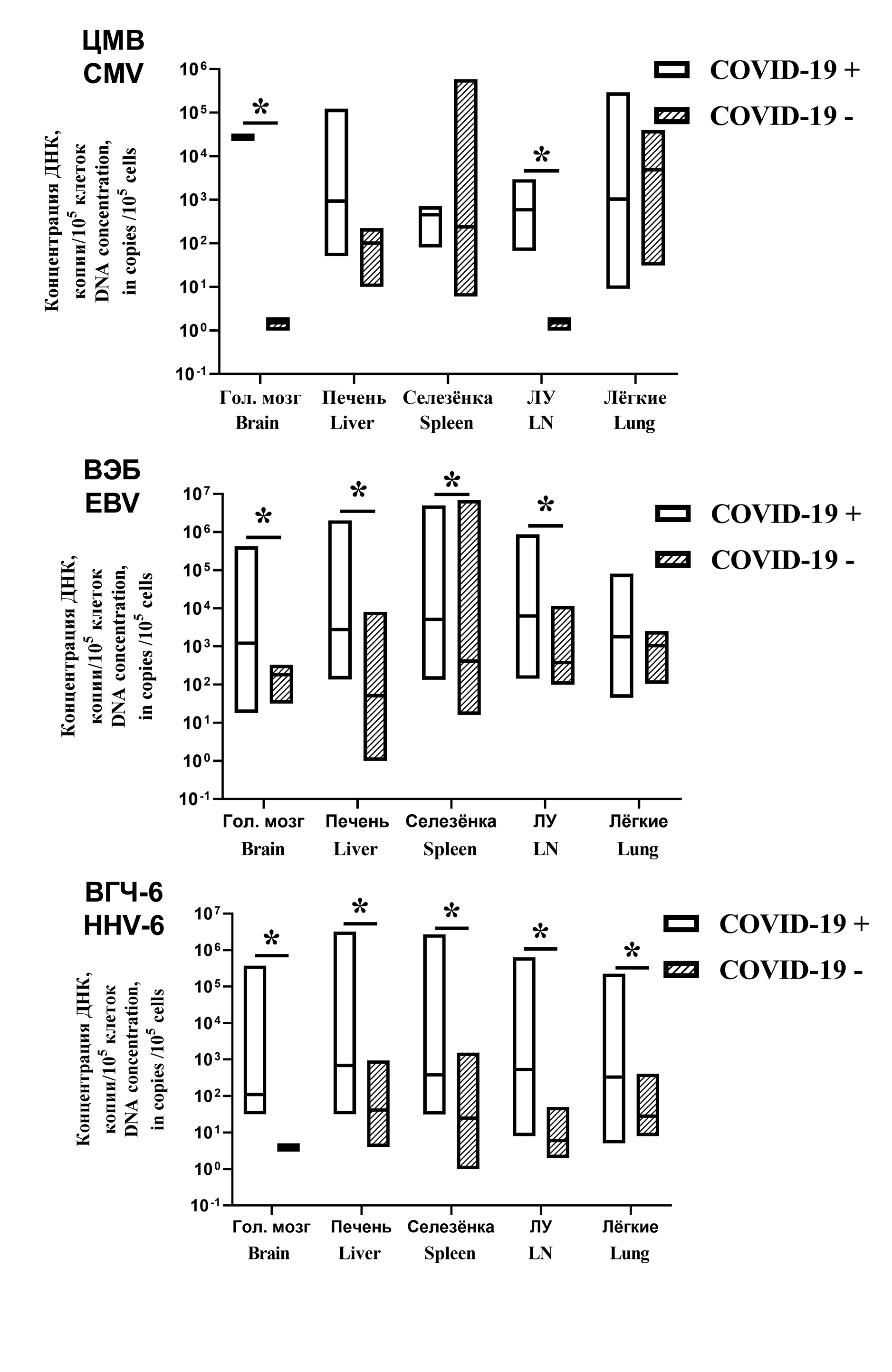
Результаты. В аутопсийных образцах ДНК ГВЧ была обнаружена у всех пациентов в обеих группах. В 1-й группе вирус Эпштейна‒Барр (ВЭБ) чаще обнаруживали в лимфоузлах (94%), вирус герпеса человека 6-го типа (ВГЧ-6) – в печени (68%), цитомегаловирус (ЦМВ) – в лимфоузлах (18%), вирус простого герпеса (ВПГ) – в головном мозге (16%), вирус варицелла-зостер (ВЗВ)– в легких и селезенке (по 3%). Различия в частоте встречаемости ГВЧ между группами были статистически незначимыми. Важные различия установлены при анализе вирусной нагрузки. У 1-й группы количество проб, содержавших более 1000 копий ДНК ГВЧ на 100 тыс. клеток, составляло 52,4%, во 2-й группе – 16,6% (p < 0,002). Установлена ассоциация между реактивацией ВПГ и ВГЧ-6 и тяжестью поражения легких. Активация ВЭБ коррелировала с повышением уровней ферментов печени.
Заключение. Полученные результаты свидетельствует о реактивации ГВЧ у пациентов с летальным исходом COVID-19. Обнаружение ГВЧ ассоциировалось с тяжелыми повреждениями легких и печени, что указывает на связь реактивации ГВЧ со смертельными исходами COVID-19.
Полный текст
Открыть статью на сайте журналаОб авторах
Кирилл Иванович Юрлов
ФГБУ «Национальный исследовательский центр эпидемиологии и микробиологии имени Н.Ф. Гамалеи» Минздрава России
Email: kir34292@yandex.ru
ORCID iD: 0000-0002-4694-2445
SPIN-код: 1767-5652
научный сотрудник
Россия, 123098, МоскваСофья Александровна Якушина
ФГБУ «Национальный исследовательский центр эпидемиологии и микробиологии имени Н.Ф. Гамалеи» Минздрава России; ГБУЗ «Инфекционная клиническая больница № 1 ДЗМ»
Email: sofia.iakushina@gmail.com
ORCID iD: 0000-0003-0507-0174
SPIN-код: 9585-8019
младший научный сотрудник, врач-инфекционист
Россия, 123098, Москва; 125367, МоскваНаталья Евгеньевна Федорова
ФГБУ «Национальный исследовательский центр эпидемиологии и микробиологии имени Н.Ф. Гамалеи» Минздрава России
Email: ninani@mail.ru
ORCID iD: 0000-0001-8466-7993
SPIN-код: 1090-2763
кандидат биол. наук, ведущий научный сотрудник
Россия, 123098, МоскваЛидия Борисовна Кистенева
ФГБУ «Национальный исследовательский центр эпидемиологии и микробиологии имени Н.Ф. Гамалеи» Минздрава России; ГБУЗ «Инфекционная клиническая больница № 1 ДЗМ»
Email: lidia.kisteneva@gmail.com
ORCID iD: 0000-0001-7336-409X
SPIN-код: 9205-3670
доктор мед. наук, ведущий научный сотрудник
Россия, 123098, Москва; 125367, МоскваЕлена Ивановна Келли
ГБУЗ «Инфекционная клиническая больница № 1 ДЗМ»
Email: ekelly@yandex.ru
ORCID iD: 0009-0000-2718-9462
врач-патологоанатом
Россия, 125367, МоскваАлександр Алексеевич Каниболоцкий
ГБУЗ «Научно-исследовательский институт скорой помощи им. Н.В. Склифосовского ДЗМ»; ГБУ «Научно-исследовательский институт организации здравоохранения и медицинского менеджмента ДЗМ»
Email: dr.kaa@mail.ru
ORCID iD: 0000-0001-6123-8387
SPIN-код: 3976-1662
Scopus Author ID: 57223849355
ResearcherId: HLG-3242-2023
кандидат мед. наук, доцент, заведующий патологоанатомическим отделением НИИ СП им. Н.В. Склифосовского ДЗМ, заведующий ОМО по патологической анатомии ГБУ «НИИОЗММ ДЗМ»
Россия, 129090, Москва; 115184, МоскваЕвгений Николаевич Ивкин
ГБУЗ «Научно-исследовательский институт скорой помощи им. Н.В. Склифосовского ДЗМ»; ГБУ «Научно-исследовательский институт организации здравоохранения и медицинского менеджмента ДЗМ»
Email: evgenuivkin@rambler.ru
ORCID iD: 0009-0004-2609-1788
врач-патологоанатом НИИ СП им. Н.В. Склифосовского ДЗМ, специалист ОМО по патологической анатомии ГБУ «НИИОЗММ ДЗМ»
Россия, 129090, Москва; 115184, МоскваНаталья Александровна Антипят
ГБУЗ «Инфекционная клиническая больница № 1 ДЗМ»
Автор, ответственный за переписку.
Email: natadog70@bk.ru
ORCID iD: 0000-0001-8578-2838
заместитель главного врача по медицинской части
Россия, 125367, МоскваИгорь Николаевич Тюрин
ГБУЗ «Инфекционная клиническая больница № 1 ДЗМ»
Email: tyurin.dti@yandex.ru
ORCID iD: 0000-0002-5696-1586
SPIN-код: 6755-0576
главный врач
Россия, 125367, МоскваВиктор Филиппович Ларичев
ФГБУ «Национальный исследовательский центр эпидемиологии и микробиологии имени Н.Ф. Гамалеи» Минздрава России
Email: vlaritchev@mail.ru
ORCID iD: 0000-0001-8262-5650
SPIN-код: 5826-1430
доктор мед. наук, ведущий научный сотрудник
Россия, 123098, МоскваНаталья Андреевна Демидова
ФГБУ «Национальный исследовательский центр эпидемиологии и микробиологии имени Н.Ф. Гамалеи» Минздрава России
Email: ailande@yandex.ru
ORCID iD: 0000-0003-1961-9789
SPIN-код: 8759-0277
научный сотрудник
Россия, 123098, МоскваЕкатерина Ивановна Леснова
ФГБУ «Национальный исследовательский центр эпидемиологии и микробиологии имени Н.Ф. Гамалеи» Минздрава России
Email: wolf252006@yandex.ru
ORCID iD: 0000-0002-2801-6843
SPIN-код: 9901-8607
научный сотрудник
Россия, 123098, МоскваРегина Рафаиловна Климова
ФГБУ «Национальный исследовательский центр эпидемиологии и микробиологии имени Н.Ф. Гамалеи» Минздрава России
Email: rklimova@yandex.ru
ORCID iD: 0000-0002-4147-8444
SPIN-код: 8286-6108
кандидат биол. наук, старший научный сотрудник
Россия, 123098, МоскваОльга Владимировна Масалова
ФГБУ «Национальный исследовательский центр эпидемиологии и микробиологии имени Н.Ф. Гамалеи» Минздрава России
Email: ol.mas@mail.ru
ORCID iD: 0000-0001-5571-5669
SPIN-код: 7210-0870
доктор биол. наук, ведущий научный сотрудник, заведующая лабораторией
Россия, 123098, МоскваАлла Александровна Кущ
ФГБУ «Национальный исследовательский центр эпидемиологии и микробиологии имени Н.Ф. Гамалеи» Минздрава России
Email: vitallku@mail.ru
ORCID iD: 0000-0002-3396-5533
SPIN-код: 6964-1715
доктор биол. наук, профессор, ведущий научный сотрудник
Россия, 123098, МоскваСписок литературы
- Carvalho J.L., Silva-Carvalho A.E., Garcez E.M., Saldanha-Araujo F. Commentary: mesenchymal stem cells: a new piece in the puzzle of COVID-19 treatment. Front. Immunol. 2021; 12: 682195. https://doi.org/10.3389/fimmu.2021.682195
- Rabi F.A., Al Zoubi M.S., Kasasbeh G.A., Salameh D.M., Al-Nasser A.D. SARS-CoV-2 and coronavirus disease 2019: what we know so far. Pathogens. 2020; 9(3): 231. https://doi.org/10.3390/pathogens9030231
- Blanco-Melo D., Nilsson-Payant B.E., Liu W.C., Uhl S., Hoagland D., Møller R., et al. Imbalanced host response to SARS-CoV-2 drives development of COVID-19. Cell. 2020; 181(5): 1036–45.e9. https://doi.org/10.1016/j.cell.2020.04.026
- Montazersaheb S., Hosseiniyan Khatibi S.M., Hejazi M.S., Tarhriz V., Farjami A., Ghasemian Sorbeni F., et al. COVID-19 infection: an overview on cytokine storm and related interventions. Virol. J. 2022; 19(1): 92. https://doi.org/10.1186/s12985-022-01814-1
- Lowery S.A., Sariol A., Perlman S. Innate immune and inflammatory responses to SARS-CoV-2: Implications for COVID-19. Cell Host Microbe. 2021; 29(7): 1052–62. https://doi.org/10.1016/j.chom.2021.05.004
- Liu L., Wei Q., Lin Q., Fang J., Wang H., Kwok H., et al. Anti-spike IgG causes severe acute lung injury by skewing macrophage responses during acute SARS-CoV infection. JCI Insight. 2019; 4(4): e123158. https://doi.org/10.1172/jci.insight.123158
- Zheng M., Gao Y., Wang G., Song G., Liu S., Sun D., et al. Functional exhaustion of antiviral lymphocytes in COVID-19 patients. Cell Mol. Immunol. 2020; 17(5): 533–5. https://doi.org/10.1038/s41423-020-0402-2
- Wang Y., Zheng J., Islam M.S., Yang Y., Hu Y., Chen X. The role of CD4+FoxP3+ regulatory T cells in the immunopathogenesis of COVID-19: implications for treatment. Int. J. Biol. Sci. 2021; 17(6): 1507–20. https://doi.org/10.7150/ijbs.59534
- Thorne L.G., Reuschl A.K., Zuliani-Alvarez L., Whelan M.V.X., Turner J., Noursadeghi M., et al. SARS-CoV-2 sensing by RIG-I and MDA5 links epithelial infection to macrophage inflammation. EMBO J. 2021; 40(15): e107826. https://doi.org/10.15252/embj.2021107826
- Cantan B., Luyt C.E., Martin-Loeches I. Influenza infections and emergent viral infections in intensive care unit. Semin. Respir. Crit. Care Med. 2019; 40(4): 488–97. https://doi.org/10.1055/s-0039-1693497
- Talan L., Akdemir Kalkan İ., Altıntaş N.D., Yörük F. Cytomegalovirus reactivation in critically-ill COVID-19 patients. Balkan Med. J. 2022; 39(4): 301–2. https://doi.org/10.4274/balkanmedj.galenos.2022.2022-2-2
- Amaral P.H., Ferreira B.M., Roll S., Neves P.D., Pivetta L.G., Mohrbacher S., et al. COVID-19 and cytomegalovirus co-infection: a challenging case of a critically ill patient with gastrointestinal symptoms. Eur. J. Case Rep. Intern. Med. 2020; 7(10): 001911. https://doi.org/10.12890/2020_001911
- Bernal K.D.E., Whitehurst C.B. Incidence of Epstein-Barr virus reactivation is elevated in COVID-19 patients. Virus Res. 2023; 334: 199157. https://doi.org/10.1016/j.virusres.2023.199157
- Manoharan S., Ying L.Y. Epstein Barr virus reactivation during COVID-19 hospitalization significantly increased mortality/death in SARS-CoV-2(+)/EBV(+) than SARS-CoV-2(+)/EBV(-) patients: a comparative meta-analysis. Int. J. Clin. Pract. 2023; 2023: 1068000. https://doi.org/10.1155/2023/1068000
- Berzero G., Campanini G., Vegezzi E., Paoletti M., Pichiecchio A., Simoncelli A.M., et al. Human herpesvirus 6 encephalitis in immunocompetent and immunocompromised hosts. Neurol. Neuroimmunol. Neuroinflamm. 2021; 8(2): e942. https://doi.org/10.1212/NXI.0000000000000942
- Di Nora A., Pizzo F., Costanza G., Ruggieri M., Falsaperla R. Human herpes 6 encephalitis in co-infection with COVID-19. Acta Neurol. Belg. 2023; 123(2): 687–8. https://doi.org/10.1007/s13760-022-01961-w
- Katz J., Yue S., Xue W. Herpes simplex and herpes zoster viruses in COVID-19 patients. Ir. J. Med. Sci. 2022; 191(3): 1093–7. https://doi.org/10.1007/s11845-021-02714-z
- Shafiee A., Teymouri Athar M.M., Amini M.J., Hajishah H., Siahvoshi S., Jalali M., et al. Reactivation of herpesviruses during COVID-19: A systematic review and meta-analysis. Rev. Med. Virol. 2023; 33(3): e2437. https://doi.org/10.1002/rmv.2437
- Nakashima J., Kadomatsu Y., Itagaki S., Otani T., Kiriu T., Matsunaga A., et al. A case-series of six autopsy cases of COVID-19 including three cases of cytomegalovirus coinfection. Pathol. Int. 2022; 72(6): 358–60. https://doi.org/10.1111/pin.13230
- Haslbauer J.D., Zinner C., Stalder A.K., Schneeberger J., Menter T., Bassetti S., et al. Vascular damage, thromboinflammation, plasmablast activation, T-cell dysregulation and pathological histiocytic response in pulmonary draining lymph nodes of COVID-19. Front. Immunol. 2021; 12: 763098. https://doi.org/10.3389/fimmu.2021.763098
- Iqbal B., Rahman N.M., Hallifax R.J. COVID-19-related pleural diseases. Semin. Respir. Crit. Care Med. 2023; 44(4): 437–46. https://doi.org/10.1055/s-0043-1769616
- Paolucci S., Cassaniti I., Novazzi F., Fiorina L., Piralla A., Comolli G., et al. EBV DNA increase in COVID-19 patients with impaired lymphocyte subpopulation count. Int. J. Infect. Dis. 2021; 104: 315–9. https://doi.org/10.1016/j.ijid.2020.12.051
- Simonnet A., Engelmann I., Moreau A.S., Garcia B., Six S., El Kalioubie A., et al. High incidence of Epstein-Barr virus, cytomegalovirus, and human-herpes virus-6 reactivations in critically ill patients with COVID-19. Infect. Dis. Now. 2021; 51(3): 296–9. https://doi.org/10.1016/j.idnow.2021.01.005
- Chen T., Song J., Liu H., Zheng H., Chen C. Positive Epstein-Barr virus detection in coronavirus disease 2019 (COVID-19) patients. Sci. Rep. 2021; 11(1): 10902. https://doi.org/10.1038/s41598-021-90351-y
- Meng M., Zhang S., Dong X., Sun W., Deng Y., Li W., et al. COVID-19 associated EBV reactivation and effects of ganciclovir treatment. Immun. Inflamm. Dis. 2022; 10(4): e597. https://doi.org/10.1002/iid3.597
- Giacconi R., Cardelli M., Piacenza F., Pierpaoli E., Farnocchia E., Di Rosa M., et al. Effect of cytomegalovirus reactivation on inflammatory status and mortality of older COVID-19 patients. Int. J. Mol. Sci. 2023; 24(7): 6832. https://doi.org/10.3390/ijms24076832
- Pérez-Granda M.J., Catalán P., Muñoz P., Aldámiz T., Barrios J.C., Ramírez C., et al. Cytomegalovirus reactivation in patients diagnosed with severe COVID-19: A point prevalence study in a general hospital. Rev. Esp. Quimioter. 2023; 36(1): 45–51. https://doi.org/10.37201/req/068.2022
- Pérez-Pedrero Sánchez-Belmonte M.J., Sánchez-Casado M., Moran Gallego F.J., Piza Pinilla R., Gomez Hernando C., Paredes Borrachero I. Herpes simplex virus type 1 (HSV-1) over-infection in patients with acute respiratory distress syndrome secondary to COVID-19 pneumonia: Impact on mortality. Med. Clin. (Engl. Ed). 2023; 160(2): 66–70. https://doi.org/10.1016/j.medcle.2022.04.019
- Yang X., Yu Y., Xu J., Shu H., Xia J., Liu H., et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir. Med. 2020; 8(5): 475–81. https://doi.org/10.1016/S2213-2600(20)30079-5
- Li Q., Chen Z., Zhou X., Li G., Zhang C., Yang Y. Ferroptosis and multi-organ complications in COVID-19: mechanisms and potential therapies. Front. Genet. 2023; 14: 1187985. https://doi.org/10.3389/fgene.2023.1187985
- Gabrielli L., Balboni A., Borgatti E.C., Virgili G., Petrisli E., Cantiani A., et al. Inherited chromosomally integrated human herpesvirus 6: laboratory and clinical features. Microorganisms. 2023; 11(3): 548. https://doi.org/10.3390/microorganisms11030548
- Qiu M.Z., He C.Y., Lu S.X., Guan W.L., Wang F., Wang X.J., et al. Prospective observation: Clinical utility of plasma Epstein-Barr virus DNA load in EBV-associated gastric carcinoma patients. Int. J. Cancer. 2020; 146(1): 272–80. https://doi.org/10.1002/ijc.32490
- Соломай Т.В., Семененко Т.А., Филатов Н.Н., Ведунова С.Л., Лавров В.Ф., Смирнова Д.И. и др. Реактивация инфекции, вызванной вирусом Эпштейна–Барр (Herpesviridae: Lymphocryptovirus, HHV-4), на фоне COVID-19: эпидемиологические особенности. Вопросы вирусологии. 2021; 66(2): 152–61. https://doi.org/10.36233/0507-4088-40 https://elibrary.ru/nhbzyr
- Roncati L., Manenti A., Fabbiani L., Malagoli C., Nasillo V., Lusenti B., et al. HSV1 viremia with fulminant hepatitis as opportunistic sequela in severe COVID-19. Ann. Hematol. 2022; 101(1): 229–31. https://doi.org/10.1007/s00277-021-04417-y
- Silaghi-Dumitrescu R., Patrascu I., Lehene M., Bercea I. Comorbidities of COVID-19 patients. Medicina (Kaunas). 2023; 59(8): 1393. https://doi.org/10.3390/medicina59081393
- Nikitskaya E., Lebedeva A., Ivanova O., Maryukhnich E., Shpektor A., Grivel J.C., et al. Cytomegalovirus-productive infection is associated with acute coronary syndrome. J. Am. Heart Assoc. 2016; 5(8): e003759. https://doi.org/10.1161/JAHA.116.003759
- Chimenti C., Verardo R., Grande C., Francone M., Frustaci A. Infarct-like myocarditis with coronary vasculitis and aneurysm formation caused by Epstein-Barr virus infection. ESC Heart Fail. 2020; 7(3): 938–41. https://doi.org/10.1002/ehf2.12611
- Chen X., Li Y., Deng L., Wang L., Zhong W., Hong J., et al. Cardiovascular involvement in Epstein-Barr virus infection. Front. Immunol. 2023; 14: 1188330. https://doi.org/10.3389/fimmu.2023.1188330
- Prasoppokakorn T., Assanasen T., Chantranuwatana P., Suankratay C. EBV-associated lymphoid interstitial pneumonia in IBD patient: Case report and literature review. Respir. Med. Case Rep. 2020; 30: 101059. https://doi.org/10.1016/j.rmcr.2020.101059
- Yurlov K.I., Masalova O.V., Kisteneva L.B., Khlopova I.N., Samokhvalov E.I., Malinovskaya V.V., et al. Human herpesviruses increase the severity of hepatitis. Biology (Basel). 2021; 10(6): 483. https://doi.org/10.3390/biology10060483
- Lin J., Zheng Y., Zhao N., Cui F., Wu S. Herpesvirus latent infection promotes stroke via activating the OTUD1/NF-κB signaling pathway. Aging (Albany NY). 2023; 15(17): 8976–92. https://doi.org/10.18632/aging.205011.
- Verma D., Church T.M., Swaminathan S. Epstein-Barr virus lytic replication induces ACE2 expression and enhances SARS-CoV-2 pseudotyped virus entry in epithelial cells. J. Virol. 2021; 95(13): e0019221. https://doi.org/10.1128/JVI.00192-21
- Perera M.R., Greenwood E.J.D., Crozier T.W.M., Elder E.G., Schmitt J., Crump C.M., et al. Human cytomegalovirus infection of epithelial cells increases SARS-CoV-2 superinfection by upregulating the ACE2 receptor. J. Infect. Dis. 2023; 227(4): 543–53. https://doi.org/10.1093/infdis/jiac452
- Yu X., Li L., Chan M.T.V., Wu W.K.K. Bioinformatic analyses suggest augmented interleukin-17 signaling as the mechanism of COVID-19-associated herpes zoster. Environ. Sci. Pollut. Res. Int. 2021; 28(46): 65769–75. https://doi.org/10.1007/s11356-021-15567-x
- Naendrup J.H., Garcia Borrega J., Eichenauer D.A., Shimabukuro-Vornhagen A., Kochanek M., Böll B. Reactivation of EBV and CMV in severe COVID-19-epiphenomena or trigger of hyperinflammation in need of treatment? A large case series of critically ill patients. J. Intensive Care Med. 2022; 37(9): 1152–8. https://doi.org/10.1177/08850666211053990
- Yang E.V., Webster Marketon J.I., Chen M., Lo K.W., Kim S.J., Glaser R. Glucocorticoids activate Epstein Barr virus lytic replication through the upregulation of immediate early BZLF1 gene expression. Brain Behav. Immun. 2010; 24(7): 1089–96. https://doi.org/10.1016/j.bbi.2010.04.013
Дополнительные файлы