Seroprevalence of Anti-Mpox Virus IgG Antibody and Awareness of Mpox Disease in Ibadan, Southwest Nigeria
- Authors: Olayiwola J.1, Akagbosu A.1, Samson O.1, Alaba A.1, Aponjolosun B.1, Soyemi S.2
-
Affiliations:
- Ajayi Crowther University
- University College Hospital, Ibadan
- Issue: Vol 70, No 5 (2025)
- Pages: 463-470
- Section: ORIGINAL RESEARCHES
- URL: https://ogarev-online.ru/0507-4088/article/view/353629
- DOI: https://doi.org/10.36233/0507-4088-337
- EDN: https://elibrary.ru/spvndn
- ID: 353629
Cite item
Full Text
Abstract
Purpose. Mpox cases were previously common in children; recent outbreaks of clade II have mostly affected young adults. Therefore, this study examines the knowledge, attitudes, and seroprevalence of the Mpox virus among consenting participants in Ibadan.
Materials and methods. Eligible individuals were those who voluntarily participated in the study and met the inclusion criteria specified for the study. A cross-sectional survey was conducted involving 94 respondents, investigating socio-demographic factors, awareness levels, attitudes toward prevention, and infection rates. The anti-Mpox virus IgG antibody was detected quantitatively using the Enzyme-Linked Immunosorbent Assay (ELISA) technique. The data were then analyzed using the χ2 test, while the antibody quantification was displayed with a Box and Whisker plot; statistical significance was determined at p < 0.05.
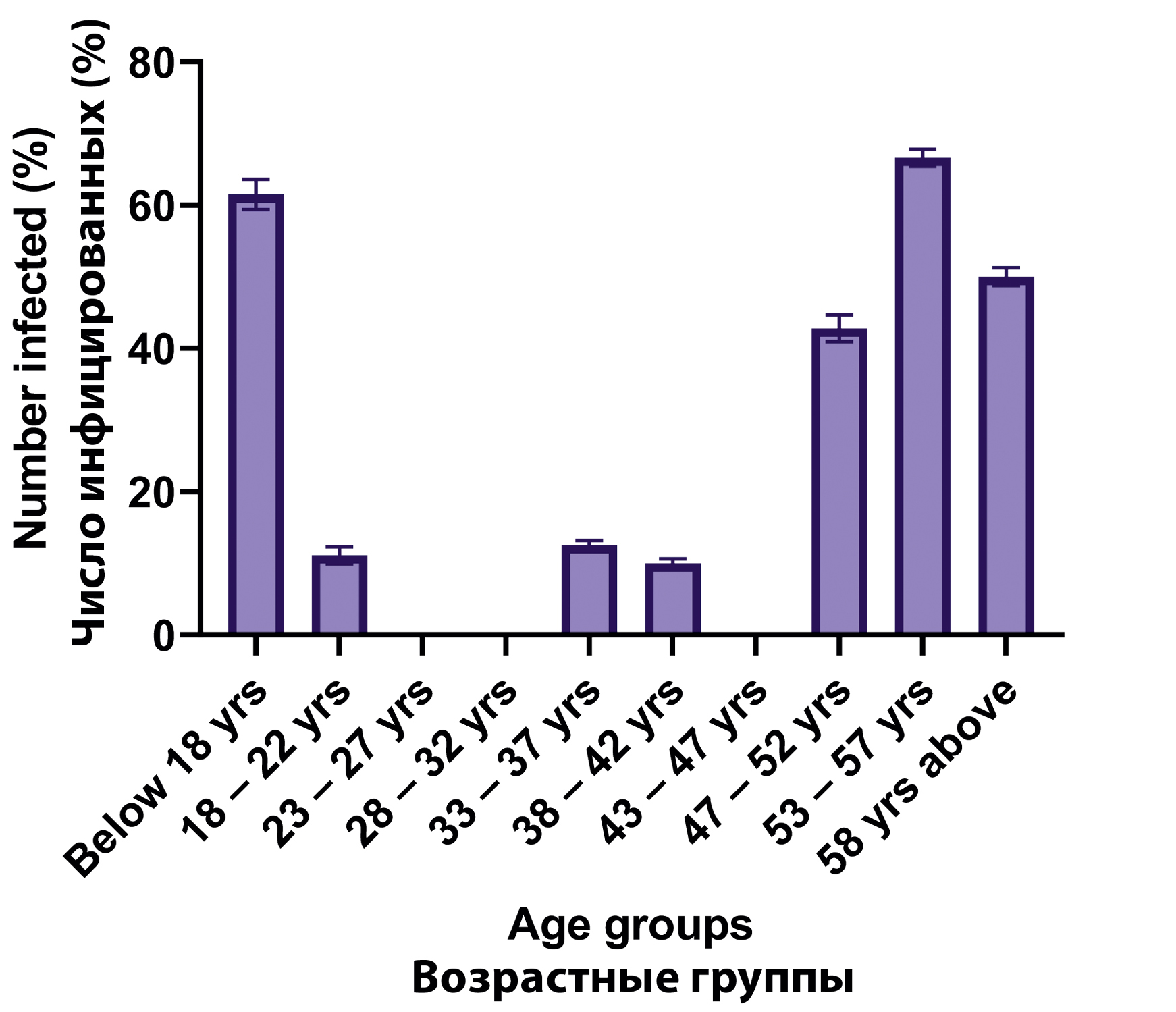
Results. The majority of respondents were female (66.7%) and aged 58 years and above (20.0%). Most had tertiary (40.0%) and secondary education (34.4%). Awareness of the Mpox was moderate, with 61.1% having heard of the virus, primarily through news (20.0%) and healthcare workers (18.9%). However, knowledge gaps were evident: only 38.9% recognized symptoms, and 40.0% understood modes of transmission. Attitudes towards prevention were generally positive; 60.0% believed Mpox could be prevented, and 73.3% were willing to take a vaccine. Still, readiness to engage in screening was low; 81.1% had never been tested, and 58.9% were unaware of local test availability. Regarding seroprevalence, females showed a significantly higher infection rate (27.4%) than males (9.6%) (χ2 = 3.854, p = 0.050). Age-wise, the highest infection rates occurred in those < 18 years (61.5%) and 53–57 years (66.6%) (χ2 = 30.817, p = 0.000), indicating significant age-related differences.
Conclusion. The findings highlight the need for targeted public health education, increased test access, and focused intervention strategies to improve Mpox virus prevention and control, especially among vulnerable age groups and under-informed populations.
Keywords
Full Text
##article.viewOnOriginalSite##About the authors
John Olusola Olayiwola
Ajayi Crowther University
Author for correspondence.
Email: jo.olayiwola@acu.edu.ng
ORCID iD: 0000-0003-2919-0154
Ph. D, Senior Lecturer, Medical Microbiology Unit, Department of Microbiology and Biotechnology
Nigeria, OyoAdesuwa Oluwatofunmi Akagbosu
Ajayi Crowther University
Email: Adesuwaakagbosu8@gmail.com
ORCID iD: 0009-0004-0499-6308
B Sc., Laboratory Technologist, Medical Microbiology Unit, Department of Microbiology and Biotechnology
Nigeria, OyoOyindamola John Samson
Ajayi Crowther University
Email: jo.samson@acu.edu.ng
ORCID iD: 0000-0003-0404-7634
M Sc., Assistant Lecturer, Environmental Microbiology Unit, Department of Microbiology and Biotechnology
Nigeria, OyoAdemola Emmanuel Alaba
Ajayi Crowther University
Email: ae.alaba@acu.edu.ng
ORCID iD: 0000-0002-4152-9803
M Sc., Lecturer II, Medical Microbiology Unit, Department of Microbiology and Biotechnology
Nigeria, OyoBabalola Sunday Aponjolosun
Ajayi Crowther University
Email: bs.aponjolosun@acu.edu.ng
ORCID iD: 0000-0002-7736-8474
Ph. D, Lecturer II, Environmental Microbiology Unit, Department of Microbiology and Biotechnology
Nigeria, OyoStephen Ademola Soyemi
University College Hospital, Ibadan
Email: dcrown1martyr@gmail.com
ORCID iD: 0000-0002-3997-1213
M Sc., Research Officer I, PAOOS Diagnostic Centre, Department of Pathology
Nigeria, IbadanReferences
- Wassenaar T.M., Wanchai V., Ussery D.W. Comparison of Monkeypox virus genomes from the 2017 Nigeria outbreak and the 2022 outbreak. J. Appl. Microbiol. 2022; 133(6): 3690–8. https://doi.org/10.1111/jam.15806
- Harapan H., Ophinni Y., Megawati D., Frediansyah A., Mamada S.S., Salampe M., et al. Monkeypox: a comprehensive review. Viruses. 2022; 14(10): 2155. https://doi.org/10.3390/v14102155
- Mauldin M.R., Andrea M.M., Yoshinori J.N., Anna M., Erin R.W., Whitni D., et al. Exportation of Monkeypox virus from the African continent. J. Infect. Dis. 2022; 225(8): 1367–76. https://doi.org/10.1093/infdis/jiaa559
- Bunge E.M., Bernard H., Liddy C., Florian L., Heinz W., Lorraine R.B., et al. The changing epidemiology of human monkeypox—a potential threat? A systematic review. PLoS Negl. Trop. Dis. 2022; 16(2): e0010141. https://doi.org/10.1371/journal.pntd.0010141
- Nguyen P.Y., Ajisegiri W.S., Costantino V., Chughtai A.A., MacIntyre C.R. Reemergence of human monkeypox and declining population immunity in the context of urbanization, Nigeria, 2017–2020. Emerg. Infect. Dis. 2021; 27(4): 1007–14. https://doi.org/10.3201/eid2704.203569
- Kabuga A.I., El Zowalaty M.E. A review of the monkeypox virus and a recent outbreak of skin rash disease in Nigeria. J. Med. Virol. 2019; 91(4): 533–40. https://doi.org/10.1002/jmv.25348
- Reed K.D., Melski J.W., Graham M.B., Regnery R.L., Sotir M.J., Wegner M.V., et al. The detection of Monkeypox in humans in the Western Hemisphere. N. Engl. J. Med. 2004; 350(4): 342–50. https://doi.org/10.1056/nejmoa032299
- Yinka-Ogunleye A., Aruna O., Dalhat M., Ogoina D., McCollum A., Disu Y., et al. (2019). Outbreak of human Monkeypox in Nigeria in 2017-18: a clinical and epidemiological report. Lancet Infect. Dis. 2019; 19(8): 872–9. https://doi.org/10.1016/s1473-3099(19)30294-4
- Kuebel C., Haskett E. “I’m doing the best I can”: teaching general music in the time of COVID-19. Update Univ. S. C. Dep. Music. 2023; 41(2): 28–37. https://doi.org/10.1177/87551233211067766
- Thornhill J.P., Antinori A., Orkin C.M. Monkeypox virus infection across 16 countries – April-June 2022. Reply. N. Engl. J. Med. 2022; 387(25): e69. https://doi.org/10.1056/nejmc2213969
- WHO. Investigations ongoing into atypical cases of Monkeypox now reported in eight countries in Europe; 2022.
- Ogoina D., Iroezindu M., James H.I., Olumide A.I., Omoleke S., Yinka-Ogunleye A. Monkeypox outbreaks in Nigeria: Epidemiological and clinical features, public health response, and implications for the future. Lancet Infect. Dis. 2022; 22(10): e234–43.
- Bunge E.M., Hoet B., Chen L., Lienert F., Weidenthaler H., Baer L.R. The changing epidemiology of human monkeypox-A potential threat? A systematic review. PLoS Negl. Trop. Dis. 2022; 16(2): e0010141. https://doi.org/10.1371/journal.pntd.0010141
- McQuiston J.H., Braden C.R., Bowen M.D., McCollum A.M., McDonald R., Carnes N., et al. The CDC domestic mpox response – United States, 2022–2023. MMWR Morb. Mortal Wkly Rep. 2023; 72(20): 547–52. https://doi.org/10.15585/mmwr.mm7220a2
- Sharif N., Nazmul S., Khalid J.A., Ibrahim F.H., Fuad M.A., Isabel D., et al. Molecular epidemiology, transmission and clinical features of 2022-mpox outbreak: a systematic review. Health Sci. Rep. 2023; 6(10): e1603. https://doi.org/10.1002/hsr2.1603
- Ogoina D., Inestol O., Adesola Y.O., Chikwe I., Nnaemeka N., Olusola A. Case report: recurrent mpox in a healthcare worker in Nigeria. Am. J. Trop. Med. Hyg. 2023; 109(4): 858–60. https://doi.org/10.4269/ajtmh.23-0232
- Olojede O., Bakare D., Sogbesan A., Salako J., and AA, B. An assessment of awareness, knowledge and perception of monkeypox (mpox) disease among internet users in Nigeria: a cross-sectional survey. Babcock Univ. Med. J. 2024; 7(2): 98–107. https://doi.org/10.38029/babcockuniv.med.j..v7i2.402
- Awoyomi O.J., Njoga E.O., Jaja I.F., Oyeleye F.A., Awoyomi P.O., Ibrahim M.A., et al. Mpox in Nigeria: Perceptions and knowledge of the disease among critical stakeholders-Global public health consequences. PLoS One. 2023; 18(3): e0283571. https://doi.org/10.1371/journal.pone.0283571
- Al-Mustapha A.I., Ogundijo O.A., Sikiru N.A., Kolawole B., Oyewo M., El-Nadi H., et al. A cross-sectional survey of public knowledge of the monkeypox disease in Nigeria. BMC Public Health. 2023; 23(1): 591. https://doi.org/10.1186/s12889-023-15398-0
- Bakare D., Salako J., Sogbesan A., Olojede O.E., Bakare A.A. Assessment of the level of awareness, knowledge, and risk perception of community members about mpox infection in Nigeria. Ann. Ib. Postgrad. Med. 2024; 22(1): 76–87.
- WHO. WHO delivering on its commitment to protect and improve people’s health: stories of healthier populations, access to services and emergency response; 2024.
- Ghazy R.M., Yazbek S., Gebreal A., Hussein M., Addai S.A., Mensah E., Sarfo M., et al. Monkeypox vaccine acceptance among Ghanaians: a call for action. Vaccines (Basel). 2023; 11(2): 240. https://doi.org/10.3390/vaccines11020240
- Ogoina D, Mahmmod M.D., Ballah A.D., Mildred O., Nneka M.C.I., Sebastine O.O., et al. Mpox epidemiology and risk factors, Nigeria, 2022. Emerg. Infect. Dis. 2024; 30(9): 1799–808. https://doi.org/10.3201/eid3009.240135
- Mauldin M.R., McCollum A.M., Nakazawa Y.J., Mandra A., Whitehouse E.R., Davidson W., et al. Exportation of monkeypox virus from the African continent. J. Infect. Dis. 2022; 225(8): 1367–76. https://doi.org/10.1093/infdis/jiaa559
Supplementary files